Focal epileptic seizure in a young female from South Korea
Fokální epileptický záchvat u mladé ženy z Jižní Korey
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors:
M. Kesslerová; I. Štětkářová; Z. Svobodová; T. Peisker
Authors‘ workplace:
University Hospital Královské Vinohrady
; Prague, Czech Republic
; Department of Neurology, Third Faculty, of Medicine, Charles University and
Published in:
Cesk Slov Neurol N 2020; 83/116(3): 330-331
Category:
Letter to Editor
doi:
https://doi.org/10.14735/amcsnn2020330
Overview
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Dear editors,
We would like to share with you a rare case of neurocysticercosis observed in a young foreign female in whom the disease manifested with a focal epileptic seizure [1]. Neurocysticercosis is extremely rare in Europe, but common in South Asia or South America, and it is one of the most probable epileptogenic lesions in India [2].
We present the case of a 35-year-old female patient from South Korea with no history of any diseases. When she was going to the toilet at about midnight, her right hand started shaking, she felt rhythmic twitching of the hand, experienced distortion of her face, and allegedly she could not breathe for a while. Subsequently, she felt weakness in her right upper limb for a short time. She did not fall unconscious. She never experienced any such problems before.
The objective baseline neurological finding showed no phatic disorder (clinical examination was limited given the language barrier) and no pathological topical neurological finding was present; the patient’s tongue was slightly bitten.
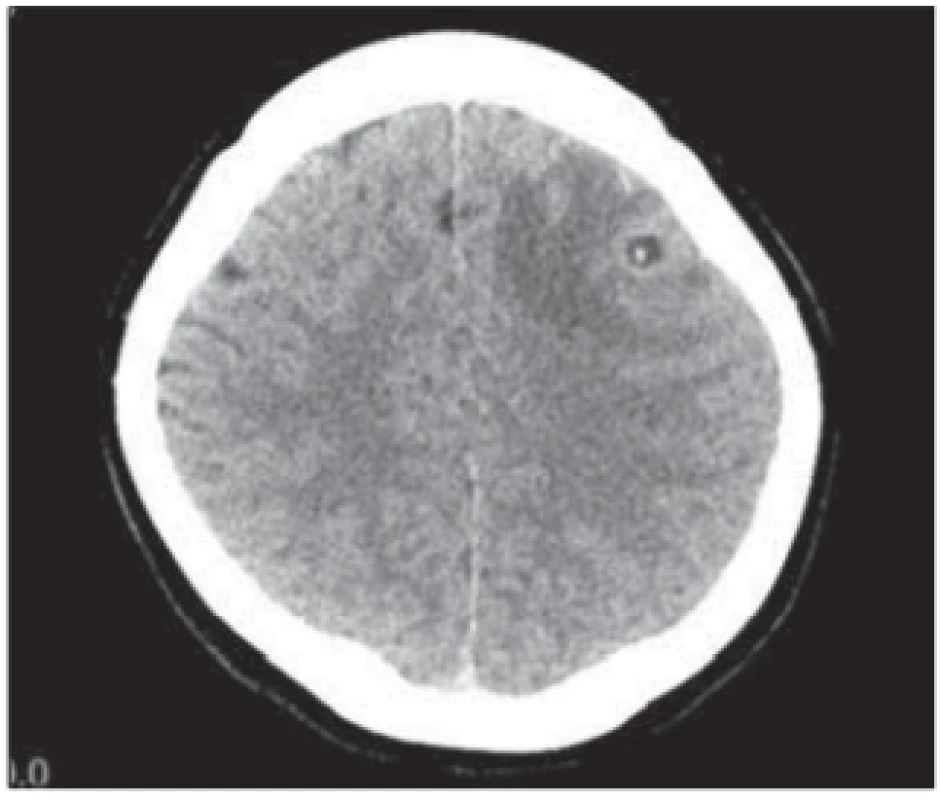
Acute laboratory assessments (blood serum) showed no remarkable findings. EEG showed a lower amplitude and no indications of epileptiform pattern. CT imaging of the brain indicated a round-shaped hypodense lesion in the left frontal region, sized 7 mm, with central dot-like hyperdensity and vasogenic oedema. The lesion could correspond to neurocysticercosis (Fig. 1). MRI of the brain showed a cystic ring enhancing lesion in the left frontal region, so far with no regressive changes in terms of calcifications, with distinct perifocal oedema; most likely a granular nodular stage of neurocysticercosis (Fig. 2). CT imaging of the neck, chest, abdomen, and pelvis showed no findings of lymphoproliferation and no cystic or tumorous changes.
Obr. 1. CT mozku, transverzální řez. Kulovité hypodenzní ložisko frontálně vlevo
velikosti 7 mm, s centrální tečkovitou hyperdenzitou odpovídá neurocysticerkóze.
Obr. 2. MR mozku, transverzální řezy. Cystické ložisko frontálně vlevo s enhancujícím prstencem, s výrazným perifokálním edémem. Nejspíše granulárně nodulární stadium neurocystercerkózy. (a) T1 vážený snímek; (b) T2 vážený snímek; (c) T1 vážený snímek s gadoliniem.
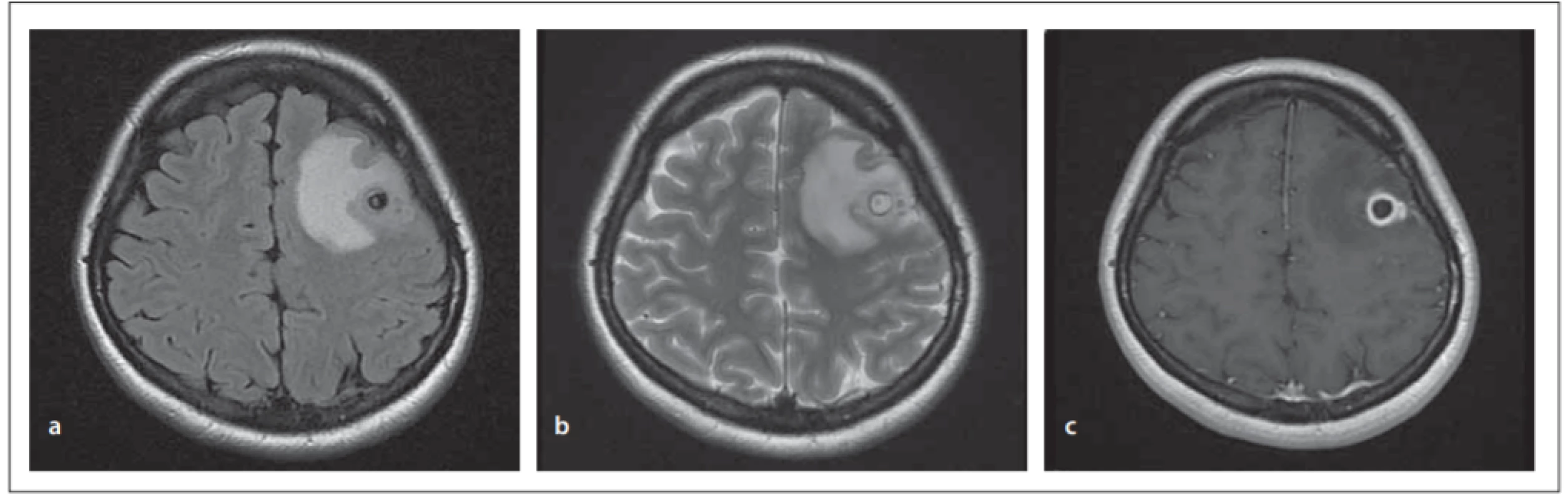
Based on the clinical and morphological presentation (CT and MRI of the brain), the condition was diagnosed as neurocysticercosis in the left cerebral hemisphere, manifesting as a focal motor epileptic seizure.
Antiepileptic therapy was administered during hospitalization – levetiracetam 250 mg twice daily with a gradual increase of the dose, and antiedematous therapy – mannitol and corticosteroids. No additional epileptic seizure occurred.
Upon agreement with the National Reference Laboratory, we collected serum samples for tissue helminthoses (serologic evidence of cysticercosis) testing of which was negative. The patient was transferred to the Department of Infectious and Tropical Diseases at Na Bulovce Hospital where she received specific treatment with albendazole and antiedematous therapy in the duration of 2 weeks. Follow-up MRI of the brain 2 weeks later showed a stationary cystic formation in the left frontal region with a small-sized internal nodule and partial regression of the vasogenic oedema; the finding corresponded to the colloidal vesicular stage of neurocysticercosis.
The patient returned to South Korea. We have no information about her further fate.
Cysticercosis is caused by the tapeworm Taenia solium whose larval stage induces cysticercosis in humans [3]. In recent years, the incidence of taeniosis/cysticercosis in the Czech Republic is very low; the total amount of about 10 cases in 1990–2017 [4].
Humans can become infected by consuming eggs of Taenia solium by faecal-oral route, e. g., from infected water or food, but also through autoinfection. Cysticerci can occur in many organs, most commonly in the central nervous system, eye, heart or muscles, and in the subcutaneous connective tissue. Clinical symptoms depend on the localization and amount of cysticerci.
Neurocysticercosis is the most serious form [5]; the cysticerci are found in the brain cortex, subarachnoid space, and brain ventricles.
The most common signs include epileptic seizures, intracranial hypertension, meningoencephalitis, or mental disorders. It strongly depends on the number, location, size and evolutionary stage of the lesions, and on the inflammatory response of the host.
Neurocysticercosis has four anatomical stages (vesicular, vesicular-coloidal, granular-nodular, nodular-calcified). The most epileptogenic one is the 2nd stage when the cysticercus dies. Neurocysticercosis is a major contributor to the burden of seizure disorders and epilepsy also in most of the world [2,6] as it was observed in our patient. The disease can be diagnosed based on the presence of antibodies in the serum (ELISA, Western-blot methods). The diagnosis of sporadic larvae is difficult because only low levels of the antibodies are produced. In such a case, the cysticerci can be detected using imaging methods (CT, MRI) that provide relatively typical images [7]. The blood count may also be altered (eosinophilia). The therapy is based on antiparasitic drugs (albendazole, praziquantel); however, this therapy may worsen the inflammation around the cysticercus. If the treatment is ineffective or associated with such complications, surgery needs to be approached.
Disclosures
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Prof. Ivana Stetkarova, MD, PhD
Department of Neurology Third Faculty of Medicine Charles University and University Hospital Královské Vinohrady
Šrobárova 1150/50
100 34 Prague
Czech Republic
e-mail: ivana.stetkarova@fnkv.cz
Accepted for review: 9. 4. 2020
Accepted for print: 8. 1. 2020
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2020 Issue 3
-
All articles in this issue
- Primary progressive aphasia
- Are we close to targeted treatments for Huntington’s disease? YES
- Are we close to targeted treatments for Huntington’s disease? NO
- Are we close to targeted treatments for Huntington’s disease? COMMENT
- Cognitive disorders in children with epilepsy
- Autoimmune encephalitis with negative anti-neuronal antibodies – clinical characteristics and available methods of antibody detection
- APOE and BDNF as genetic risk markers for predicting the onset and development of cognitive deficits due to Alzheimer’s disease
- Role of novel laboratory techniques in Niemann-Pick type C disease diagnostics
- Headaches in pregnancy
- Occurrence and risk factors of unprovoked epileptic seizures in ischaemic stroke patients
- Validation of DYsphagia in MUltiple Sclerosis questionnaire – Czech version of DYMUS
- Effect of a neuropalliative care intervention on quality of life in patients with progressive neurological disease – interventional study
- Characteristics of a cohort of boys with Duchenne and Becker muscular dystrophies – a study from a single neuromuscular centre
- Epidural application of steroids Part 2 – The quality of life of patiens before application
- Glioblastoma grade IV – long-term survival
- Stanovisko redakční rady k diskuzi o úrovni a směřování Cesk Slov Neurol N
- Erratum
- Informace vedoucího redaktora
- Recenze
- Impact of dementia on the trajectories of quality of life in older adults
- Magnetic resonance spectroscopy metabolomics of cerebrospinal fluid in patients with multiple sclerosis, clinically isolated syndrome, other inflammatory brain diseases and controls
- Focal epileptic seizure in a young female from South Korea
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Glioblastoma grade IV – long-term survival
- Primary progressive aphasia
- Headaches in pregnancy
- Cognitive disorders in children with epilepsy
