Cavernous Malformation of the Cauda Equina – a Case Report
Kavernózní malformace kaudy equiny – kazuistika
Kavernózní angiomy kaudy equiny jsou vzácné cévní malformace; v literatuře bylo popsáno pouze 15 případů. U většiny případů malformace adherovala k míšním kořenům kaudy equiny.
Popis případu:
Je popisován případ 67letého muže s jednoměsíční historií bolesti dolní části zad vyzařující do oblasti levého ischiadiku, s exacerbací bolesti v posledním týdnu. Při neurologickém vyšetření byla zjištěna poklepová bolestivost nad lumbosakrální páteří, palpační citlivost nad levým ischiadikem, taktilní hypestezie v dermatomu L3–4 vlevo a chabá paréza levé dolní končetiny. Dále byl snížen reflex patelární a šlachy Achillovy vlevo. Magnetická rezonance odhalila nehomogenně se sytící masu obliterující míšní kanál v úrovni L2–3 a komprimující kaudu equinu. Masa, která adherovala ke kořenům a filum terminale, byla při operaci totálně resekována. Histopatologické vyšetření potvrdilo diagnózu kavernózní malformace (CM). Po operaci rychle ustoupila bolest, do šestého měsíce ustoupila i paréza a poruchy citlivosti.
Závěr:
CM kaudy equiny je extrémě vzácná léze, která se může manifestovat bolestí dolní části zad a v ischiadické oblasti, neurologickým deficitem nebo subarachnoidálním krvácením. Předoperační diferenciální diagnóza oproti intradurálnímu tumoru pouze ze zobrazovacího nálezu, zejména u případů bez krvácení, není snadná. CM je léčitelná chirurgickou excizí. Je bezpečné excidovat filum terminale nebo izolovaný kořen v případě, že k nim CM pevně adheruje.
Klíčová slova:
kavernózní malformace – angioma – vaskulární malformace – cauda equina
Authors:
Y. Yi 1; D. Zhao- xia 2; Z. Dong 1; Y. Gang 1; T. Wen- yuan 1
Authors place of work:
Department of Neurosurgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
1; Department of Intensive Care Unit, Xi’nan Hospital of The Third Military Medical University, Chongqing, China
2
Published in the journal:
Cesk Slov Neurol N 2009; 72/105(6): 575-579
Category:
Kazuistika
Summary
Background:
Cavernous angiomas of the cauda equina are rare vascular malformations; only 15 cases have been reported in the literature. Most cases described adherance to the spinal root of the cauda equina.
Case description:
A 67‑year - old male patient presented with a 1-month history of lower back pain and left sciatica and a 1‑week history of exacerbated symptoms. On neurological examination the patient was found to be tender to percussion over the lumbosacral spine, had tenderness over the left sciatic nerve, left hypoesthesia on the L3 – 4 dermatome with left flaccid lower monoparesis. In addition, he was found to have decreased patellar and Achilles’ reflexes on the left. Magnetic resonance imaging (MRI) revealed a heterogeneous enhancing mass obliterating the spinal canal at the L2 – 3 level and compressing the cauda equina. On operation the lesion was found to adhere to the filum terminale as well as the roots, and was totally resected. Pathological examination confirmed the diagnosis of a cavernous malformation (CM). The patient’s pain was quickly resolved after the operation. He remains pain‑free with full recovery of motor function and hypoesthesia in the sixth postoperative month.
Conclusion:
CMs of the cauda equina are extremely rare lesions that may present with lower back pain and sciatica, neurological deficit or subarachnoid haemorrhage. Preoperative differential diagnosis of intradural tumours is not easy in cases without haemorrhage from imaging alone. They can be successfully treated by surgical excision. It is safe to cut the filum terminale or a single root to which the lesion is adherent.
Keywords :
cavernous malformations – angioma – vascular malformations – cauda equina
Introduction
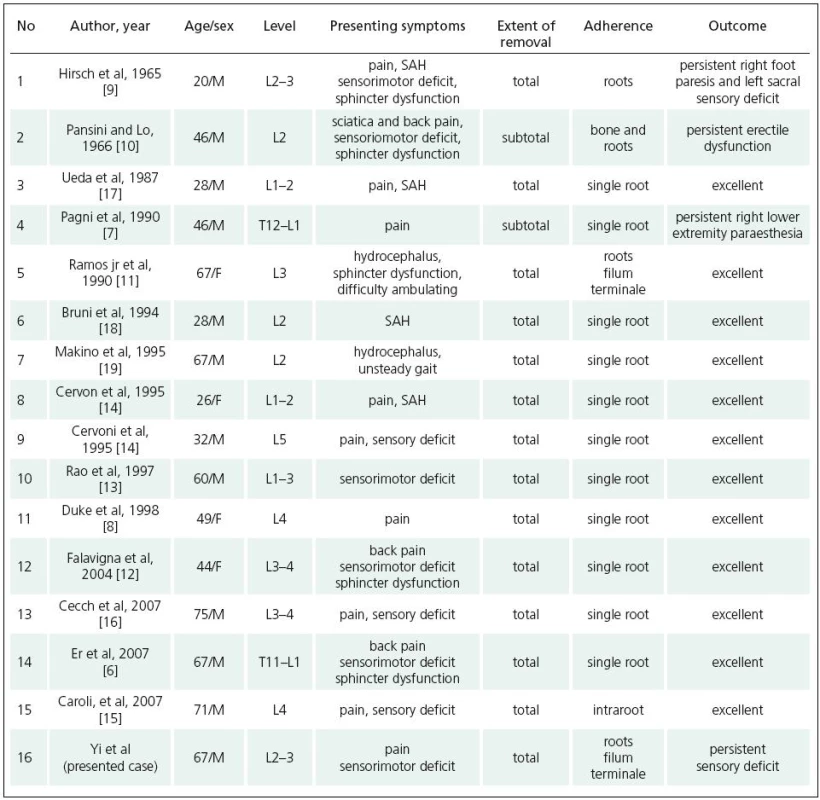
Cavernous malformations (CMs), or cavernous angiomas, are rare vascular malformations consisting of closely packed, large, sinusoid-esque vascular channels without neural or glial elements [1]. These lesions can occur throughout the central nervous system, but they favour the cerebral zone [2]. Spinal variants are most frequently found in the vertebral body [3,4]. Approximately 3% of spinal haemangiomas are intradural, and these are usually intramedullary. Only rare cases present with intradural-extramedullary involvement [5]. Although most CMs in intradural-extramedullary space are to be found in the cauda equina [6], the number of cases is still very small. To date, there have been only 15 surgically treated cases reported (Table 1). We describe an unusual case of intradural cauda equina CM adherent to roots and filum terminale. We discuss its clinical, radiological, and surgical findings, and follow with a brief review of the pertinent literature.
Case report
A 67‑year-old male patient, presenting with a 1-month history of lower back pain radiating into the posterior part of the left leg and a 1‑week history of exacerbated symptoms accompanied by numbness of left lower extremity, was admitted to the hospital. The pain was exacerbated on assuming a recumbent position and worse at night. There was no loss of bladder or bowel sphincter control, no fever and no onset of severe pain during the course.
Neurological examination revealed tenderness to percussion over the lumbar spine and tenderness over the sciatic nerve. Left tactile hypoesthesia on the L3–4 dermatome was identified, and flaccid left lower paraparesis was present with 3/5 muscle strength on plantar flexion of the left foot, difficulty in walking on tiptoe and decreased patellar and Achilles’ reflexes on the same side. Left straight leg raising test was positive. Rectogenital examination was normal.
Magnetic resonance imaging (MRI) revealed a 20 × 18mm heterogeneous enhancing mass obliterating the spinal canal at the L2–3 level and compressing the cauda equina. The lesion exhibited a mixed signal on both T1 - and T2-weighted images (Figure 1 a–c).

A bilateral L2 and partial L3 laminectomy was performed with the tense dura opened under microscopic magnification. A 20 × 18 × 13mm dark-bluish mass was identified between the adherent nerve roots, which had compressed the roots to the right side. After sharp dissection of the adherence to the roots, we found that the mass remained closely adherent to the filum terminale, which was encapsulated within the lesion. The lesion appeared to have arisen from the filum terminale. The mass was gross totally resected after cutting off the filum terminale but no requirement to sacrifice any roots emerged. Opening the lesion in vitro, various old capsular spaces and clotted blood of variable density consistent with haemorrhage of various ages were observed. Histopathological examination confirmed a CM with numerous small vessels and large, dilated sinusoidal spaces lined with a single cell layer. The vascular channels were immediately adjacent to one another, without intervening nervous tissue (Figure 2). The course of postoperative recovery was uneventful, and the patient’s pain was immediately resolved following the operation. The patient’s motor strength returned totally after three days. The patient was discharged after seven days without pain. He remains pain‑free with full recovery of motor function, normal sphincter function and stable left L3–4 dermatome hypoesthesia in the sixth postoperative month.

Review of the literature
Table 1 provides a summary of the 15 reported surgically treated cases of cauda equina CMs, including the present report. The patients are in their third to eighth decades of life. The ages of the patients are between 20 and 75 years, with an average of 49.6 years (Table 1). There is a male predominance (11 male and 5 female). The clinical symptoms were most often the result of local compression of the nerve roots of the cauda equina. Accordingly, low back pain with sciatica was the major symptom in twelve cases, while two cases among them presented with only pain [7,8]. Sensorimotor deficit was revealed among seven cases [6,9–13], and three cases had only sensory deficit [14–16]. Five patients had loss of sphincter control [6,9–12]. Subarachnoid haemorrhage was observed in four of the cases [4,14,17,18]. Two cases of cavernous angioma in the cauda equina diagnosed on the basis of headache due to hydrocephalus were reported [11,19]. Intraoperatively, all cases were found to be adherent to the nerve roots, among which twelve adhered to a single root and four to more roots. Additionally, one cavernoma was found to have invaded from extradural space and to be adherent to the vertebral body [10]; one other lesion originated from between roots [15]. Adherence of the filum terminale to the lesions was observed in only two cases [11], including the present one. Total excision was achieved in 14 cases with preservation of neural tissue, and incomplete resection was performed in two cases in which the lesion was tightly adherent to the spinal cord [7,10]. Twelve cases recovered excellently postoperatively, while exceptions included three cases with stable sensory deficit [7,9] and one case with persistent erectile dysfunction [10].
Discussion
Cavernous angiomas are vascular malformations composed of abnormal, dilated and packed vascular sinusoidal channels without interposed neural tissue or tumour tissue. Thus they have been classified as a vascular malformation and termed cavernous malformation (CM). The most common location of these vascular malformations is the supratentorial cerebral parenchyma [2]. Only 5–16% of CMs have been reported for the spine, usually located within the vertebral bodies [12]. The cauda equina nerve root is a more rare location. CM of the cauda equina was first reported by Hirsch et al in 1965 [9]. The patient presented with pain, SAH, sensorimotor deficit and sphincter dysfunction, and diagnosis was made through operation and pathohistological study. Later, Pansini et al described a second case with operative treatment and pathological diagnosis [10]. Although these vascular malformations are discovered most frequently because of the widespread use of MRI, CMs of this location still remain uncommon lesions. A PubMed search identified just 15 cases, including the present one (Table 1).
Although CMs belong to one group of occult vascular malformations in terms of embryology and aetiology, the causation of this lesion was not clear. CMs are well demarcated. lesions. They may arise from blood vessels of the nerve roots, the inner surface of the dura mater, and the pial surface of the spinal cord. Accordingly, close adherence of the lesion to the spinal nerve roots or spinal cord have been observed during operations. In all of the cases, the cavernoma was adherent to single or multiple roots, and in three cases, the root was encapsulated within the lesion. In the current case, we observed a CM tightly adherent to the filum terminale as well as to multiple roots; we had to cut off the filum terminale in order to resect the lesion totally. Reviewing the literature, only one case with adherence to the filum terminale was reported [11]. The filum terminale is an extension structure of spinal cord without neural tissue, and it is rare to observe vessels there. Therefore, we assumed that the two latter CMs most probably originated from vessels near to the filum terminale. Another possible explanation is that the lesions in these two cases encased the structure.
Pain, sensorimotor deficit and sphincter dysfunction are common presentations for patients with CMs [6,8,15]. However, they play only a minor role in the differential diagnosis with other lesions of the cauda equina, such as schwannomas and meningiomas. We should pay more attention to the five cases with SAH. The clinical deterioration seen in these patients is thought to be secondary to repeated haemorrhage within the lesion or subarachnoid spaces. This is the most dangerous presentation among cases of CM. Given the tendency of these lesions toward haemorrhage and neurological deterioration, and that acute compressive injury to neural tissue is usually much more severe than the chronic, complete surgical resection should be performed promptly. In the present case, although there was no SAH to be observed clinically and operatively, haemorrhage within the CM was identified by opening the lesion.
MRI is the imaging modality of choice for diagnosing CMs [20,21]. The typical MRI features are those of a well‑defined lesion with mixed signal intensity on both T1 - and T2-weighted images. The mixed signal demonstrates the subacute and chronic haemorrhage within the CM [22]. CMs are often surrounded by a hypointense ring on T2-weighted images arising from haemosiderin deposition [3]. Enhancement with Gadolinium is variable [23]. Spinal myxopapillary ependymomas often present as exophytic masses at the conus and cauda equina; MRI scans show a homogeneous mass isointense on T1, hyperintense on T2 and enhancement after gadolinium. Thus it is not very difficult to distinguish these two entities preoperatively. However, among those CMs lacking the characteristic surrounding lower signal ring, the preoperative radiological diagnosis of CM is not easy, because a heterogeneous lesion signal is also generated by other disorders, such as spinal intradural tumours, spinal vascular pathologies, and infections. Spinal angiography does not reveal these lesions [13]. In the present case, we found a round lesion with heterogeneous signal intensity on T1 - and T2-weighted image and significant enhancement after injection of contrast medium. However, we found no phenomenon of hemosiderin deposition, probably because the haemorrhage was only within the CM.
The treatment of choice is surgical removal. The lesions are usually well demarcated and total excision has proved possible in most cases, including the present one, even though the lesions were closely attached to nerve roots. The most frequent surgical finding is that the lesion adheres to the nerve roots [6,8]. Most of the surgically treated cases have had excellent results, but in patients with severe preoperative neurological deficits, such as sphincter dysfunction, recovery was not complete [9,10]. Total excision was achieved in most of the cases. Subtotal removal was performed in only two cases in which the cavernoma had invaded the bone, dura and roots [10]. In most cases, the nerve root was spared when the lesions were removed, but sometimes this is not possible because the lesion originates within the nerve root [15]. In this event, even when it proved necessary to cut the single root, the patient still made a good recovery. In the present case, the cavernous angioma was adherent to the filum terminale as well as multiple roots. A similar pattern of growth is reported in only one other case [11]. We preserved all the adhering roots but cut the filum terminale because of its tight adherence to the lesion. That it is safe to cut this structure is demonstrated by the good postoperative recovery.
Conclusions
CMs of the cauda equina are extremely rare. They may initially present as low back pain, neurological deficits, or as a subarachnoid haemorrhage. The clinical outcome depends largely on the patient’s preoperative neurological status, and optimal treatment is surgical resection. In those cases in which total resection proves difficult because of tight adherence of a single root or the filum terminale to the lesions, it is safe to sacrifice the filum terminale or a single root in order to complete removal of the lesion.
Yan Yi, M.D.
The First Affiliated Hospital
of Chongqing Medical University Chongqing 400016
e‑mail:
yanyi2005@gmail.com
Accepted for review: 10. 7. 2009
Accepted for publication: 21. 8. 2009
Zdroje
1. Mastronardi L, Ferrante L, Scarpinati M, Gagliardi FM, Celli P, Fortuna A. Intradural extramedullary cavernous angioma: case report. Neurosurgery 1991; 29(6): 924 – 926.
2. Brown RD. Epidemiology and natural history of vascular malformations of the central nervous system. In: Jafar JJ, Awad IA, Rosenwasser RH (eds). Vascular Malformations of the Central Nervous System. Philadelphia: Lippincott Williams & Wilkins 1999 : 129 – 148.
3. Fontaine S, Melanson D, Cosgrove R, Bertrand G. Cavernous hemangiomas of the spinal cord: MR imaging. Radiology 1988; 166(3): 839 – 841.
4. Harrison MJ, Eisenberg MB, Ullman JS, Oppenheim JS,Camins MB, Post KD. Symptomatic cavernous malformations affecting the spine and spinal cord. Neurosurgery 1995; 37(2): 195 – 204.
5. Zevgaridis D, Medele RJ, Hamburger C, Steiger HJ, Reulen HJ. Cavernous haemangiomas of the spinal cord. A review of 117 cases. Acta Neurochir (Wien) 1999; 141(3): 237 – 245.
6. Er U, Yigitkanli K, Simsek S, Adabag A, Bavbek M. Spinal intradural extramedullary cavernous angioma: case report and review of the literature. Spinal Cord 2007; 45(9): 632 – 636.
7. Pagni CA, Canavero S, Forni M. Report of a cavernoma of the cauda equina and review of the literature. Surg Neurol 1990; 33(2): 124 – 131.
8. Duke BJ, Levy AS, Lillehei KO. Cavernous angiomas of the cauda equina: case report and review of the literature. Surg Neurol 1998; 50(5): 442 – 445.
9. Hirsch JF, Pradat P, David M. Angiomes caverneux dela queue de chaval. Neurochirurgie 1965; 11(4): 323 – 327.
10. Pansini A, Lo Re F. Raro caso di angiocavernoma della cauda. Mem Soc Tos Um Chir 1966; 27 : 679 – 696.
11. Ramos F jr, de Toffol B, Aesch B, Jan M. Hydrocephalus and cavernoma of the cauda equina. Neurosurgery 1990; 27(1): 139 – 142.
12. Falavigna A, Righesso Neto O, dos Santos JA, Ferraz FA. Cavernous angioma of the cauda equina: case report. Arq Neuropsiquiatr 2004; 62(2B): 531 – 534.
13. Rao GP, Bhaskar G, Hemaratnan A, Srinivas TV. Spinal intradural extramedullary cavernous angiomas: report of four cases and review of the literature. Br J Neurosurg 1997; 11(3): 228 – 232.
14. Cervoni L, Celli P, Gagliardi FM. Cavernous angioma of the cauda equina: report of two cases and review of the literature. Neurosurg Rev 1995; 18(4): 281 – 283.
15. Caroli E, Acqui M, Trasimeni G, Di SD, Ferrante L. A case of intraroot cauda equina cavernous angioma: clinical considerations. Spinal Cord 2007; 45(4): 318 – 321.
16. Cecchi PC, Rizzo P, Faccioli F, Bontempini L, Schwarz A, Bricolo A. Intraneural cavernous malformation of the cauda equina. J Clin Neurosci 2007; 14(10): 984 – 986.
17. Ueda S, Saito A, Inomori S, Kim I. Cavernous angioma of the cauda equina producing subarachnoid hemorrhage. Case report. J Neurosurg 1987; 66(1): 134 – 136.
18. Bruni P, Massari A, Greco R, Hernandez R, Oddi G, Chiappetta F. Subarachnoid hemorrhage from cavernous angioma of the cauda equina: case report. Surg Neurol 1994; 41(3): 226 – 229.
19. Makino K, Takamura H, Gotoh S, Andoh M. Cauda equina cavernous hemangioma associated with hydrocephalus – case report. No To Shinkei 1995; 47(8): 783 – 787.
20. Roncaroli F, Scheithauer BW, Krauss WE. Capillary hemangioma of the spinal cord. Report of four cases. J Neurosurg 2000; 93 (Suppl 1): 148 – 151.
21. Santoro A, Piccirilli M, Frati A, Salvati M, Innocenzi G,Ricci G et al. Intramedullary spinal cord cavernous malformations: report of ten new cases. Neurosurg Rev 2004; 27(2): 93 – 98.
22. Rigamonti D, Drayer BP, Johnson PC, Hadley MN, Zabramski J, Spetzler RF. The MRI appearance of cavernous malformations (angiomas). J Neurosurg 1987; 67(4): 518 – 524.
23. Sindou M, Gilg A, Vighetto A, Jouvet A. Cryptic angioma in the trochlear nerve. Excision of the invaded portion and successful repair with an autologous graft: case report. Neurosurgery 1992; 30(2): 255 – 258.
Štítky
Dětská neurologie Neurochirurgie NeurologieČlánek vyšel v časopise
Česká a slovenská neurologie a neurochirurgie

2009 Číslo 6
-
Všechny články tohoto čísla
- Carpal Tunnel Syndrome
- Microdialysis in Neurosurgery
- The Variants of the Catatonia
- Rett Syndrome
- Resection of Insular Gliomas – Volumetric Assessment of Radicality
- The Correlation of Transcranial Colour‑ Coded Duplex Sonography, CT Angiography and Digital Subtraction Angiography in Patients with Atherosclerotic Disorders of Cerebral Arteries in Common Clinical Practice
- Is Clinical- Diffusion Mismatch Associated with Good Clinical Outcome in Acute Stroke Patients Treated with Intravenous Thrombolysis?
- Short‑term Effects of Botulinum Toxin A and Serial Casting on Triceps Surae Muscle Length and Equinus Gait in Children with Cerebral Palsy
- Mental Nerve Neuropathy as a Manifestation of Systemic Malignancy
- Extracranial Schwannoma of the Hypoglossal Nerve – a Case Report
- Recurrent Ischemic Stroke in Systemic Sclerosis – a Case Report
- Intracranial Hematoma in Patients Receiving Warfarin – Case Reports and Recommended Therapy
- Cavernous Malformation of the Cauda Equina – a Case Report
- The International Classification of Functioning, Disability and Health (ICF) – Quantitative Measurement of Capacity and Performance
- Webové okénko
-
Analýza dat v neurologii XVIII.
O t-testu jsme ještě nenapsali vše - Šedesátiny primáře MU Dr. Milana Choce, CSc.
- Komentář k práci Brichtová et al. Malfunkce peritoneálního katétru vnitřního drenážního systému u dětí
- Vyhlášení cen České neurologické společnosti za rok 2008
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle
- The Variants of the Catatonia
- Rett Syndrome
- Mental Nerve Neuropathy as a Manifestation of Systemic Malignancy
- Carpal Tunnel Syndrome
