Analysis of 1775 Patients Treated by Percutaneous Radiofrequency Rhizotomy for Trigeminal Neuralgia
Analýza 1 775 pacientů léčených pro trigeminální neuralgii perkutánní radiofrekvenční rizotomií
Východiska:
Metody léčby klasické trigeminální neuralgie (cTN) jsou rozličné stejně jako jejich patofyziologie. Pacienti s cTN, u kterých nebyla medikamentózní léčba účinná nebo vyvolala nežádoucí účinky, jsou kandidáty chirurgické léčby.
Cíl:
Prezentace výsledků léčby 1775 pacientů s cTN léčených perkutánní radiofrekvenční rizotomií (pRFR). Je rovněž diskutován současný stav chirurgické léčby cTN.
Metodika:
V období od 1983 do 2001 bylo v Neurochirurgickém ústavu v Bělehradě metodou pRFR léčeno 1775 pacientů s onemocněním cTN. Autoři analyzovali iniciální a dlouhodobé výsledky, jako např. vliv rozličných typů cTN, dosažení faciální hypestezie po pRFR a předchozích chirurgických procedur v trigeminové oblasti na výsledky léčení.
Výsledky:
Dobrých iniciálních výsledků bylo docíleno u 96 % pacientů; recidivita po 5 letech se objevila u 21 % pacientů. Výsledky byly úspěšnější u pacientů, kteří prodělali krátkodobou, epizodickou, ostrou bolest v porovnání s těmi, jejichž bolesti zahrnovaly i složku stálé, tupé bolesti. Úvodní stupeň a doba trvání faciální hypestezie vyvolané pRFR nejen zvýšila úspěšnost ve zmírnění bolesti, ale také tíži neurologických komplikací.
Závěr:
pRFR nebo operace gamma nožem jsou doporučovány jako metody první volby v rámci chirurgické léčby pacientů s cTN. Mikrovaskulární dekomprese by měla být zvážena u mladších pacientů s jednoznačnou neuroradiologickou diagnózou neurovaskulární komprese v oblasti trigeminal root entry zone, nebo po selhání perkutánních neurochirurgických procedur.
Klíčová slova:
trigeminální neuralgie – radiofrekvenční rizotomie – rizotomie glycerolem – radiochirurgie gamma nožem – mikrovaskulární dekomprese
Authors:
E. Slavik; D. Radulović
Authors place of work:
Institute for Neurosurgery, CCS, Belgrade, Serbia
Published in the journal:
Cesk Slov Neurol N 2007; 70/103(4): 407-412
Category:
Krátké sdělení
Summary
Background:
Treatment of classic trigeminal neuralgia (cTN) has been as diverse as explanations of its pathophysiology. The patients with cTN refractory to medical treatment are candidates for surgical procedures.
Aims:
We report our results on 1775 patients treated for cTN with percutaneous radiofrequency rhizotomy (pRFR). We also discuss the current state of surgical management of cTN.
Methods:
In the period from 1983 to 2001, 1775 patients underwent pRFR for relief of cTN at the Institute of Neurosurgery in Belgrade. The authors analyzed the initial results and long-term follow - up data, such as the influence of different types of cTN, achieved facial hypesthesia after pRFR and prior trigeminal surgical procedures on the treatment outcome.
Results:
Initial positive results were obtained in 96% of the patients, while the recurrence rate after five years accounted for 21%, taking into consideration the whole series. Better results were achieved in patients with short episodic, sharp pain than in patients suffering from pain containing a more constant, throbbing component. Unfortunately, the initial degree and duration of facial hypesthesia provoked by pRFR, not only increased the success in pain relief, but also the degree of neurological complications.
Conclusion:
We recommend pRFR or gamma knife surgery (GK) as the first procedure for surgical treatment in majority of patients suffering from cTN. Microvascular decompression (MVD) should be considered for younger patients with clear radiological diagnosis of neurovascular compression at the trigeminal root entry zone or after failed percutaneous neurolytic procedures.
Key words:
trigeminal neuralgia – radiofrequency rhizotomy – glycerol rhizotomy – gamma knife radiosurgery – microvascular decompression
Introduction
cTN may be defined as a sudden usually unilateral and predominantly episodic recurrent painful disorder perceived in one or more sensory divisions of the trigeminal nerve. Its clinical features are characterized by brief paroxysms of electric shock-like, agonizing, lancinating or stabbing pain separated by pain-free intervals that may continue for days, weeks or even for years [1,2].
The attacks may be provoked by light tactile or vibratory stimulation of a trigger point located in the orofacial region. The attack is self-sustained once it starts. Results of neurological examination are almost always normal, except for discreet hypalgesia or hypesthesia in some patients [3].
Mainly affected individuals are of age 50 and older, but cTN can occur regardless of age [4].
Treatment of cTN has been as diverse as explanations of its pathophysiology. The patients suffering from cTN who had no favorable response or experienced significant side effects to medical therapy are candidates for surgical treatment. Two most conventional surgical procedures are pRFR of ganglion Gasseri and microvascular decompression (MVD) via posterior fossa craniectomy. If vascular compression of the trigeminal root entry zone was not perceived during the exploration of cerebello-pontine angle (CPA), the alternative procedure is a partial trigeminal sensory root rhizotomy (PTSR) [5].
The purpose of this study is to review our experience with pRFR in treatment of 1775 patients suffering from cTN and to discuss the possibility of other current surgical options for management of cTN.
Patients and Methods
Patients
The patient population consisted of 1775 patients (1052 female and 723 male), suffering from medically refractory cTN pain and treated by pRFR from 1983 to 2001.
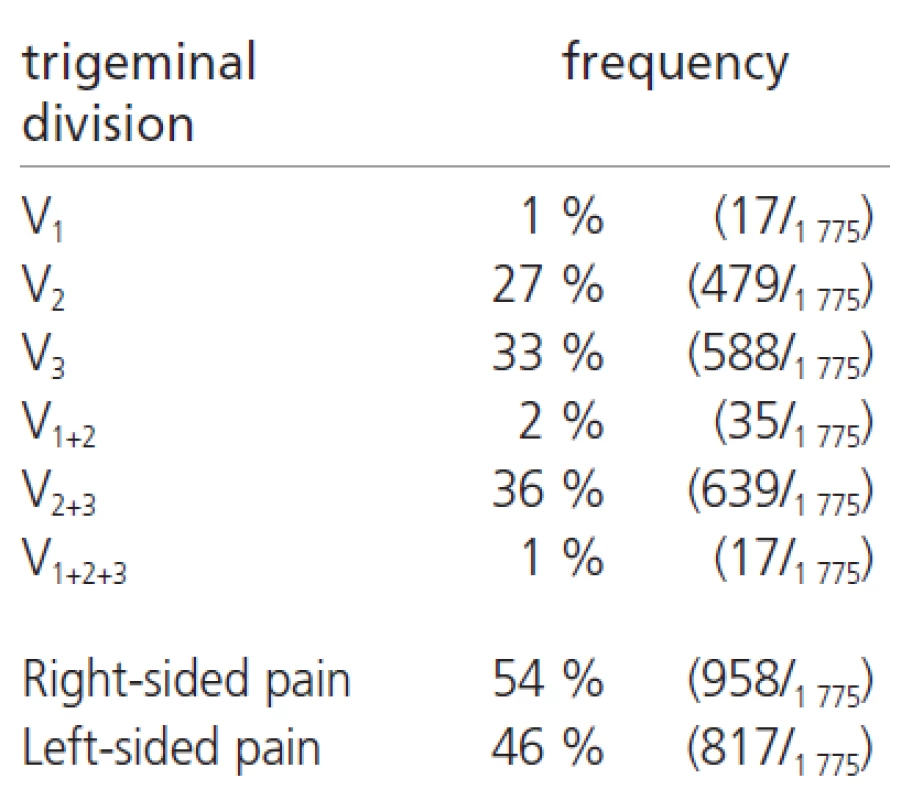
The diagnosis of cTN was based on typical clinical features. Our patients are classified in two groups according to characteristics of their pain. The patients in group A (1384/1775 ;78%) were suffering from a typical episodic, sharp or electrical shock-like, idiopathic pain lasting several seconds. The group B (391/1775 ;22%) had a component of more constant, throbbing or burning pain. Preoperative examination, computerized tomography (CT) or magnetic resonance (MRi), revealed normal findings in all patients. Neuroablative surgical procedures were previously performed on 3% of the patients (53/1775). The characteristics of the patients in this series are presented in Table1.

The pain was located on the right side in 54% of the patients, while the left side was affected in 46% of the patients. The more affected distributions were the maxillary and mandibulary nerves together (36%), as mandibulary (33%) and maxillary (27%) nerve alone (Table 2).
Methods
pRFR was conducted on sedated patient in the x-ray department under fluoroscopic guidance. We used Radionics Radiofrequency Lesion Generator model RFG-3AV and Trigeminal Neuralgia Kit Type TIC. The transbucal Hartel´s approach to the foramen ovalae was employed using submental-vertex radiographic projection [6].
Electrophysiological confirmation by low-voltage stimulation defined the exact electrode position in trigeminal ganglion. The first radiofrequency lesion was made with the electrode tip temperature of 60oC for 60 sec. Each following lesion was increased for 5oC up to 80oC with duration of 60 to 80 sec., depending on the attained analgesia and hypesthesia in the affected division. We insisted that the facial analgesia be followed by convincing moderate facial hypesthesia.
Results
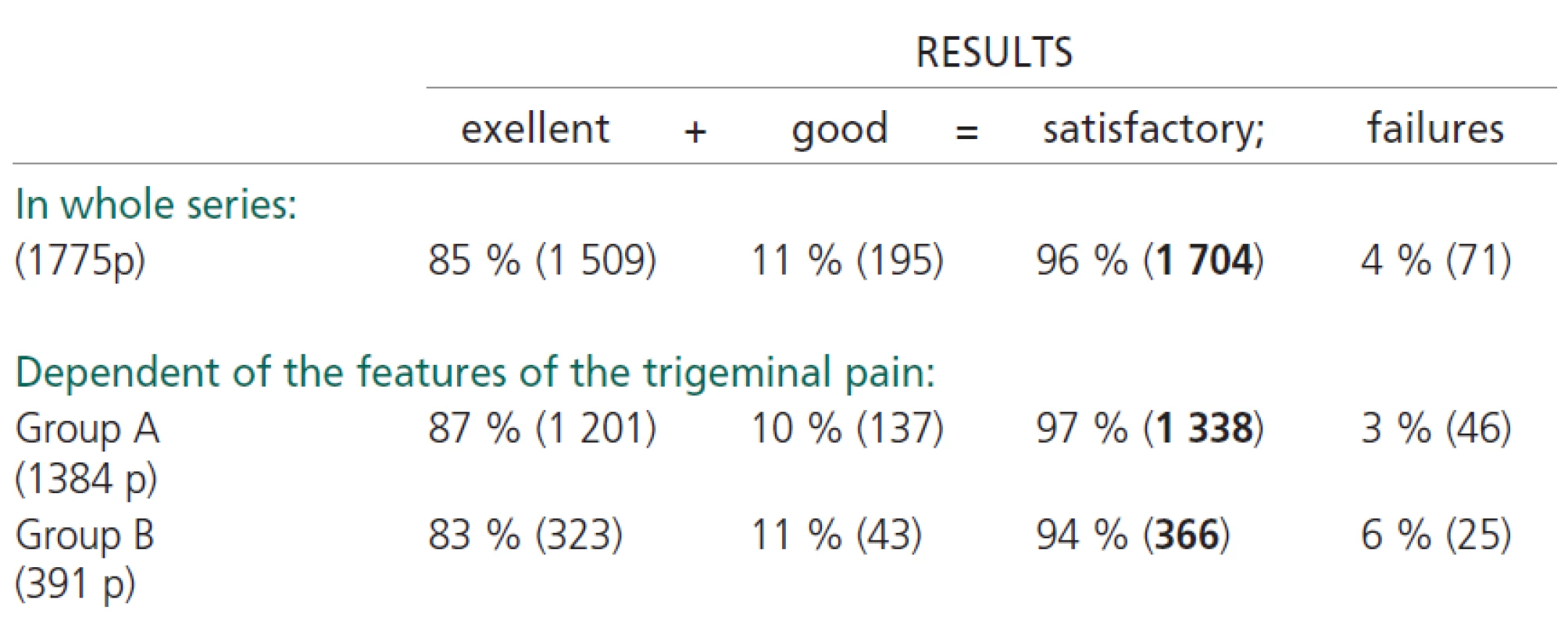
Excellent result (pain free and off medication) was obtained initially in 85% of the patients (1509/1775). Initially good result (pain free with need for medication at times) was achieved in 11% of the patients (195/1775), while an initially poor response was noted in the remaining 4% of the patients (71/1775). Excellent and good results were considered as a satisfactory outcome. The overall initially satisfactory success rate after pRFR was present in 96% of the patients (1704/1863).
According to the nature of idiopathic pain the initial success rate in group A was 97% and in group B was 94% of the cases. Table 3.
Mild facial hypesthesia after pRFR in duration of up to four weeks was present in 25% (431/1704 ) of the patients, moderate hypesthesia up to six weeks in 62% (1048/1704) of the patients, while a dense facial hypesthesia lasting more than two month was achieved in remaining 13% (225/1704 ) of the patients.
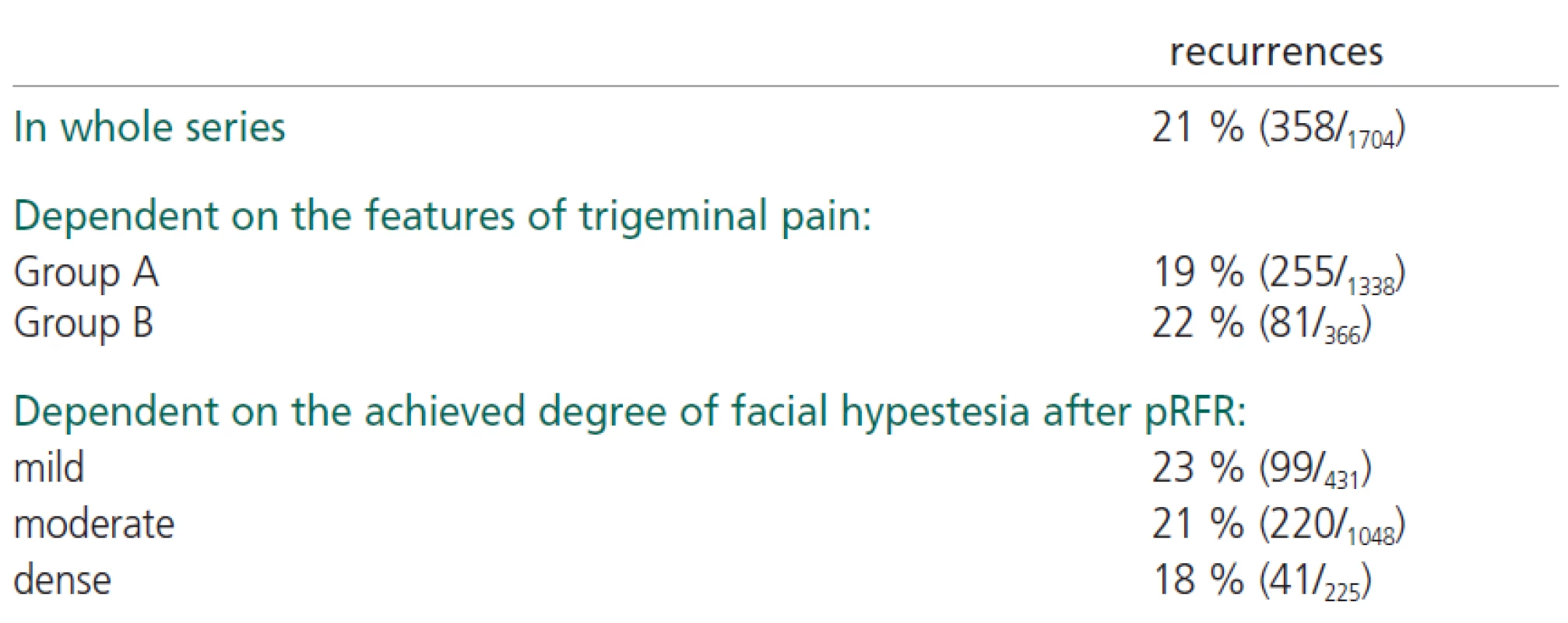
After five years the recurrence of pain in the patients with initially satisfactory results (1704 patients) accounted for 21%. This recurrence of pain was higher in group B than in group A, as in the patients with lower degree, versus higher degree, of facial hypesthesia. Table 4.
The pRFR was repeated in 283 cases with satisfactory results in 83% of the patients (235/283).
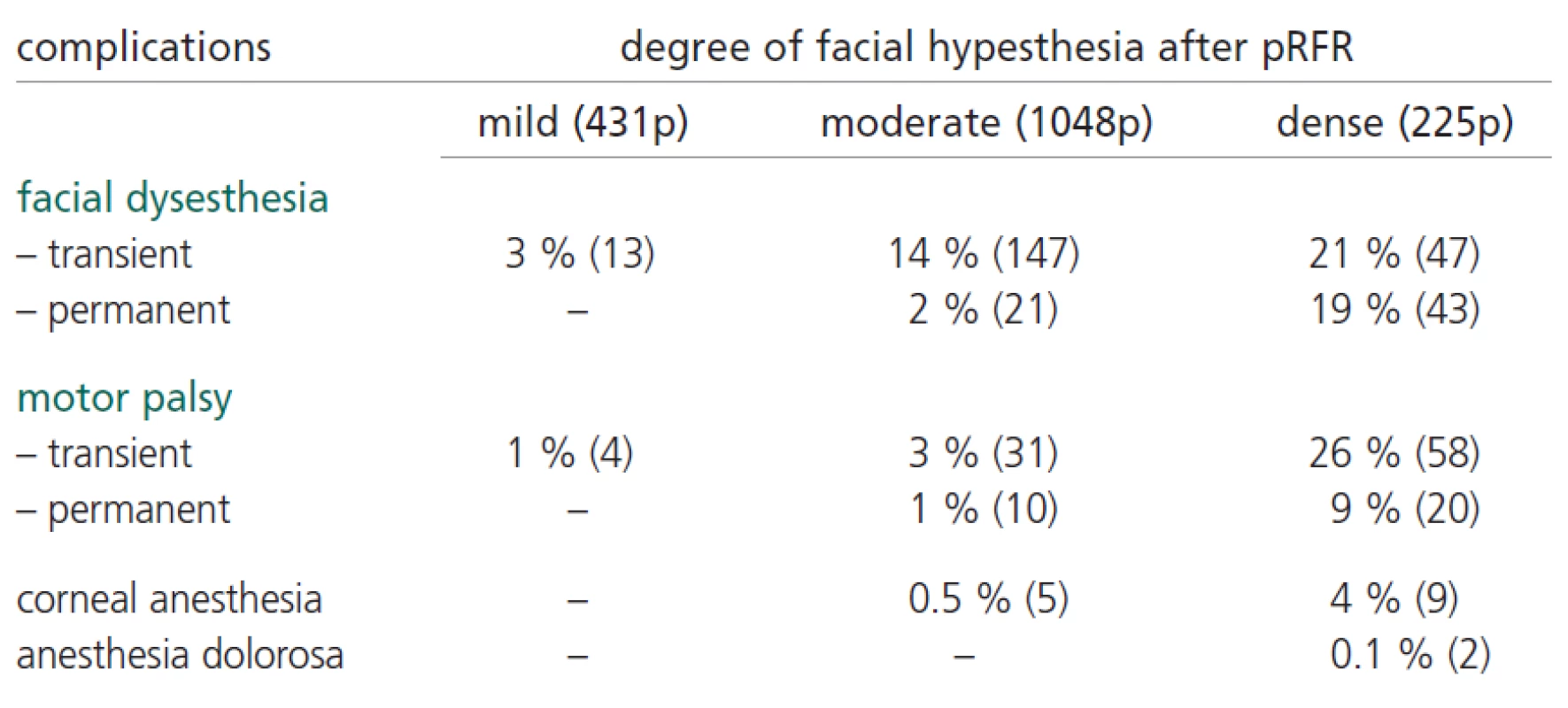
We have had no lethal outcome. As for the most frequent complications, we have noted facial dysesthesia and motor palsy. In Table 5. are presented the complications of pRFR in correlation to the degree of produced facial hypesthesia.
Discussion
As analyzed in literature, both experimental and clinical data suggest that cTN occurs in response to peripheral and central causes. The injury to the trigeminal nerve or roots causes ectopic afferent activity with a loss of inhibitory interneurons resulting in a decrease in segmental afferent inhibition. [7, 8]
If this paroxysmal activity spreads to wide dynamic range neurons on nucleus caudalis and they begin to fire at the frequency normally elicited by noxious stimuli, an attack of trigeminal neuralgia is initiated. [9]
Medically refractory cTN has been treated with a variety of surgical techniques. According to the current state the best results may be achieved by noninvasive or minimally destructive procedures on trigeminal nerve or ganglion. [10] Satisfactory pain relief for treatment of cTN can be obtained either with pRFR or percutaneous retrogasserian glycerol rhizotomy (pGlyR) or with MVD operation. Gamma knife radiosurgery has recently also emerged as a viable therapeutic option for treatment of cTN. Which of the procedure should be applied?
pRFR is a minimally invasive technique in common practice worldwide. It is used routinely and may be suggested to almost any patient. Its advantages are the avoidance of general endotracheal anesthesia, good tolerance by the elderly and the poor risk patients, reduced length of hospitalization, successful immediate and long-termed results, possibility of repeating if necessary, and low morbidity and practically no mortality. [11]
In our series, after pRFR initially satisfactory pain-relief was achieved in 96% of the patients and after a follow-up period of five years the rate of pain recurrence reached 21%. According to other reports the initial successful pain relief ranges from 91% to 98% and the pain recurrence ranges from 10% up to 80%. [12]
We noticed that the initial success and recurrence rate correlated to the degree of achieved facial hypesthesia. Therefore, the goal was to obtain moderate, but not unpleasant, sensory loss in the affected division of trigeminal nerve. Unfortunately, in cases of dense facial hypesthesia unfavorable neurological consequences were higher (facial dysesthesia, motor palsy, corneal anesthesia, anesthesia dolorosa).
There was a difference between group A and group B in the initial result and the recurrence of pain after follow-up of five years. In the group A, the initial success of pain relief was 97% and the recurrence rate accounted 19%. In group B, the initial success was lower (94%) but the recurrence rate was higher (22%). This may be explained by the new classification scheme for trigeminal neuralgia which authors theorized that the initial, thoroughly idiopathic, pain could be changed by time, obtaining discreet throbbing and more constant components, as a result of further neural injury. [13, 14]
The incidences of complications in this series (dysesthesia 12%, motor palsy 9%, corneal anesthesia 0,9% and anesthesia dolorosa 0,1%) are well in the range of published series ( dysesthesia 11-24%, motor palsy 3-25%, corneal anesthesia 0,6-20% and anesthesia dolorosa 0,2-3%). [15, 16, 17, 18, 19]
Patients previously treated by neurodestructive surgery appeared to receive less benefit from subsequent pRFR. In 53 patients with prior neuroablative operations an initial satisfactory pain relief was obtained by 84% and after five years the recurrence rate reached 26%. The patient’s age, sex, and previous response to medication had no influence on the outcome.
pGlyR is also used for treatment of cTN with the advantage of providing immediate pain relief, but with significant low long-term success rate. Reported rates of pain recurrence in the literature range up to 53% for pGLyR treated patients.19 Kondziolka in reported series with pGlyR in 1174 patients suffering from cTN noted satisfactory long-lasting pain relief in 77% of patients. [20]
GK radiosurgery is an effective and noninvasive treatment modality which has a low side effect rate. [21] Petit [22] reported the series of 112 patients with cTN who were treated with GK radiosurgery using the prescription dose of 75 Gy delivered to the involved trigeminal nerve root entry zone. After the median time to pain relief of 3 weeks, 77% of the patients experienced satisfactory pain relief. In long-term follow-up for 3 years the percent of satisfactory treatment response was 48%. Persistent trigeminal dysfunction was noted in 7,3% and bothersome facial numbness in 3,1%.
Shaya [23] treated 40 patients with medically refractory cTN with GK using the mean prescription dose of 8o Gy. At the median follow-up of 14 months 70% had satisfactory pain relief.
Rogers [24] treated 89 patients suffering from cTN with GK. The overall satisfactory pain relief from immediate to 253 days (median 63 days) was 71%. The actuarial 2.5 year pain recurrence rate for entire patient group was 36%. Complication related to partial facial sensory loss (14%).
MVD is a well established procedure. Numerous studies have revealed reliable connection between idiopathic trigeminal neuralgia and vascular compression of the trigeminal nerve. The pathophysiology of trigeminal neurovascular compression syndrome is based on the changes produced by pulsatile compression of the vessels on the nerves in the CPA. These damages, especially of myelin of large fibers, results in abnormal firing of the nerve, which has led to the ignition hypothesis. [25]
However, besides that most authorities agree with segmental demyelination as a cause of pain, how to explain the pain relief immediately after microvascular decompression ?! [26] Maybe the vascular contact with the trigeminal nerve provokes some other pathophysiological mechanisms causing seizure-like activity in the trigeminal nucleus? [21] Although the proposal that neurovascular compression is the mechanism for the production of trigeminal neuralgia is intriguing, it requires furthe7 evaluation.
Certainly, MVD should be conditioned by a clear preoperative radiological visualization of neurovascular compression at the trigeminal root entry zone. In some cases offending vessels at or near the trigeminal root entry zone may be detected by MRi without clinical manifestation of the trigeminal neuralgia. Moreover, it was demonstrated that the vascular contact at the trigeminal root entry zone exists in more than 50% of unselected necropsis, not causing the trigeminal neuralgia in all cases. [28] On the contrary, in some patients with intractable idiopathic trigeminal pain no vascular compression at trigeminal root entry zone was observed on operation. Arachnoid thickening or adhesion between the root and surrounding tissues can lead to irritation or damage to the neural tissue. [29, 30]
Finally, not all of the patients with trigeminal neuralgia could be cured by MVD. Sometimes the patients showed no response or the pain could only be alleviated to MVD. [31]
Taha and Tew [32] noted that 15% of patients who underwent craniotomy for intended MVD were found to have insignificant vascular compression or were unable to be decompressed thoroughly. In literature reported series with MVD provides the initial pain relief in up to 91-97% of patients and recurrence in up to 19% of cases. [33]
Kondo [34] reported the series of 154 patients with cTN who were treated by MVD. Immediate postoperative cure rate was 96,7%. In long-term follow-up, for more than 5 years after surgery, the satisfactory pain relief was 82,5%.
Unfortunately, MVD carries the specific risks of operations in the CPA, including the reported mortality of 1%. [35]
We also analyzed the comparative results of different surgical procedures for treatment of cTN.
Henson [19] reported the comparative results of patients treated with pGlyR and GK. The majority of pGlyR treated patients experienced a pain relief within 24 h vs, a median time to pain relief of 3 weeks with the GK radiosurgery. pGlyR has a greater facial numbness morbidity (54% vs 30%) and higher failure rate (39% vs. 24%) than GK.
Apfelbaum [12] reported the series of 702 patients surgically treated with pRFR, pGlyR and MVD. The follow-up was more than 2 years after surgery. pRFR initially produced 93% successful pain relief while in long-term follow-up obtained 81% success rate. pGlyR had 92% initial pain relief and 64% long-term success. MVD initially produced 91% success and on long-term follow-up in 81%. The initial success with all three procedures is very similar (91-93%). The long-term successes for MVD and pRFR are also equal (81%) while pGlyR has a significant lower long-term success rate (64%). Complication with pRFR and pGlyR are minimal, while with MVD could be serious or even life threatening (1% mortality). [36]
Taha and Tew [32] published the comparative results of percutaneous neurolytic procedures with MVD and GK radiosurgery. Only MVD had a mortality rate (o,6%).
Conclusions
We recommend pRFR (or GK radiosurgery) as the first procedure in treatment for medically refractory cTN in majority of cases. These procedures are especially advised for older patients or those with significant risk factors of a craniotomy.
According to our experience the pRFR may be considered for a safe, low cost procedure and easy to perform in nearly every neurosurgical center, with low complication rates and acceptable long-term results in pain relief.
Present studies suggest that the clinical features of preoperative trigeminal pain may influence the initial pain relief, as to recurrence of pain after pRFR procedure. Carefully defined moderate facial hypesthesia induced by radiofrequency lesion saves the balance between the good pain relief and low complications rate.
MVD is reserved for younger patients without significant surgical risk factors with preoperative radiological visualization of neurovascular compression at the trigeminal root entry zone or after failed percutaneous neurolytic procedures. MVD carries the specific risks of operation in CPA, including the reported mortality of 1%.
Partial sensory trigeminal root section is the surgical option in cases of negative finding on neurovascular compression during CPA exploration.
Přijato k recenzi: 10. 4. 2006
Přijato do tisku: 7. 2. 2007
prof. Eugen Slavik
Weekend N0 14
22305 Stari Banovci
Serbia
e-mail: eugens@ptt.yu
Zdroje
1. Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurg Focus 2005; 18(5): 1–3.
2. Merskey H, Bogduk N. Classification of chronic pain. Descriptors of chronic pain syndromes and definitions of pain terms. Seattle, WA: IASP Press 1994.
3. Elias WJ, Burchiel KJ. Trigeminal neuralgia and other craniofacial pain syndromes: an overview. Semin Neurosurg 2004; 15 : 59–69.
4. Fromm GJ. Pathophysiology of Trigeminal Neuralgia. In: FromM GJ, Sessle BJ, editors. Trigeminal neuralgia – Current Concepts Regarding Pathogenesis and Treatment. Boston: Butterworth-Heinemann 1991 : 106–108.
5. Cole CHD, Liu JK, Apfelbaum RI. Historical perspectives on the diagnosis and teratment of trigeminal neuralgia. Neurosurg Focus 2005; 18(5): 1–10.
6. Hartel F. Ueber die intracranielle injektionsbehandlung der trigeminusneuralgia. Med Klin 1914; 10 : 582–584.
7. Burchiel KJ. Ectopic impulse generation in focally demyelinated trigeminal nerve. Exp Neurol 1980; 69 : 423–429.
8. Burchiel KJ. Abnormal impulse generation in focally demyelinated trigeminal roots. J Neurosurg 1980; 53 : 674–683.
9. Fromm GH. Pathophysiology of Trigeminal Neuralgia. In: Fromm GH, Sessle BJ (eds). Trigeminal neuralgia – Current Concepts Regarding Pathogenesis and Treatment. Boston: Butterworth&Heinemann 1991 : 108–122.
10. Fromm GH, Sessle BJ. Summary and Conclusions. In: Fromm GH, Sessle BJ (eds). Trigeminal neuralgia – Current Concepts Regarding Pathogenesis and Treatment. Boston: Butterworth&Heinemann 1991 : 211–213.
11. Moraci A, Buonaita C, Punzo A, Parlato C, Amalfi R. Trigeminal neuralgia treated by percutaneous thermocoagulation.Comparative analysis of percutaneous thermocoagulation and other surgical procedure. Neurochirurgia (Stuttg) 1992; 35(2): 48–53.
12. Apfelbaum R. Comparison of the longterm results of microvascular decompression and percutaneous trigeminal neurolysis for the treatment of trigeminal neuralgia. International Congress Series. Elsevier Science B.V. 2002 : 629–643.
13. Burchiel KJ. A new classification for facial pain. Neurosurgery 2003; 53 : 1164–1167.
14. Burchiel KJ, Slavin KV. On the natural history of trigeminal neuralgia. Neurosurgery 2000; 46 : 152–154.
15. Siegfried J. Percutaneous controlled thermocoagulation of gasserian ganglion in trigeminal neuralgia. Experiences with 1000 cases. In: Samii J, Jannetta PJ (eds). The Cranial Nerves. Berlin: Springer-Verlag 1981 : 322–330.
16. Fraioli V, Esposito V, Guidetti B, Gruccu G, Manfredi M. Treatment of trigeminal neuralgia by thermocoagulation, glycerolization, and percutaneous compressing of the gasserian ganglion and/or retrogasserian rootles: longterm results and therapeutic protocol. Neurosurgery 1989; 24 : 239–245.
17. Moraci A, Buonaita C, Punzo A, Parlato C, Amalfi R. Trigeminal neuralgia treated by percutaneous thermocoagulation.Comparative analysis of percutaneous thermocoagulation and other surgical procedures. Neurochirurgia (Stuttg) 1992; 35(2): 48–53.
18. Tew JM, Keller JT. The treatment of trigeminal neuralgia by percutaneous radiofrequency technique. In: Keener EB (ed). Clinical Neurosurgery. Baltimore: Williams&Wilkins 1977 : 557–558.
19. Henson CF, Goldman HW, Rosenwasser RH, Downes MB, Bednarz G, Pequignot EC et al. Glycerol Rhizotomy Versus Gamma Knife Radiosurgery for the Treatment of Trigeminal Neuralgia: an Analysis of Patients Treated at one Institution. Int J Radiat Oncol Biol Phys 2005; 63 : 82–90.
20. Kondziolka D, Lunsford LD. Percutaneous retrogasseria glycerol rhizotomy for trigeminal neuralgia. Technique and expectations. Neurosurg Focus 2005; 18(5): E7.
21. Brisman R, Mooij R. Gamma Knife Radiosurgery for Trigeminal Neuralgia: Dose-volume Histograms of the Brainstem and Trigeminal Nerve. J Neurosurg 2000; 93 : 155–158.
22. Petit JH, Herman JM, Nagda S, DiBiase SJ, Chin LS. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outsomes. Int J Radiat Oncol Biol Phys 2003; 56 : 1147–1153.
23. Shaya M, Jawahar A, Caldito G, Sin A, Willis BK, Nanda A. Gamma knife radiosurgery for trigeminal neuralgia: a study of predictors of success, efficacy, safety, and outcome at LSUHSC. Surg Neurol 2004; 61 : 529–535.
24. Rogers CL, Shetter AG, Fiedler JA, Smith KA, Han PP, Speiser BL. Gamma knife radiosurgery for treatment of trigeminal neuralgia: the initial experience of the Barrow Neurological Institute. Int J Radiat Oncol Biol Phys 2000; 47 : 1013–1019.
25. Devor M, Amir E, Rappaport ZH. Pathophysiology of trigeminal neuralgia: The ignition hypothesis. Clin J Pain 2002; 18 : 4–13.
26. Leandry M, Eldrige P, Miles J. Recovery of nerve conduction following microvascular decompression for trigeminal neuralgia. Neurology 1988; 51 : 1641–1646.
27. Pagni CA. The origin of tic douloureux: A unified views. J Neurol Sci 1993; 37 : 185–194.
28. Hardy DG, Rhoton AL jr. Microsurgical relationships of the superior cerebellar artery and the trigeminal nerve. J Neurosurg 1978; 49 : 669–678.
29. Ishikawa M, Nishi S, Aoki T, Takase T, Wada E, Ohwaki H et al. Operative findings in cases of trigeminal neuralgia without vascular compression: proposal of a different mechanism. Journal of Clinical Neuroscience 2002; 9(2): 200–204.
30. Rath SA, Klein HJ, Richter HP. Findings and long-term results of subsequent operations after failed microvascular decompression for trigeminal neuralgia. Neurosurg 1996; 39 : 833–840.
31. Li ST, Pan Q, Liu N, Shen F, Liu Z, Guan Y. Trigeminal Neuralgia: What are the Important Factors for Good Operative Outcomes with Microvascular Decompression. Surg Neurol 2004; 62 : 400–405.
32. Taha JM, Tew JM. Comparisson of surgical teratments for trigeminal neuralgia: reevaluation of radiofrequency rhizotomy. Neurosurgery 1996; 38 : 865–871.
33. Jannetta PJ. Surgical Treatment: Microvascular Decompression. In: Fromm GH, Sessle BJ (eds). Trigeminal neuralgia – Current Concepts Regarding Pathogenesis and Treatment. Boston: Butterworth-Heinemann 1991 : 145–157.
34. Kondo A, Tanabe H. What should be done, what should not be done in microvascular decompression surgery. International Congress Series 1259. Elsevier 2004 : 353–356.
35. Taarnhoj P. Decomprresion of the posterior trigeminal root in trigeminal neuralgia A 30-year follow-up review. J Neurosur 1982; 57 : 14–17.
36. Maesawa S, Salame C, Flickinger JC, Pirris S, Kondziolka D, Lunsford LD. Clinical Outcomes after Stereotactic Radiosurgery for Idiopathic Trigeminal Neuralgia. J Neurosurg 2001; 94 : 14–20.
Štítky
Dětská neurologie Neurochirurgie NeurologieČlánek vyšel v časopise
Česká a slovenská neurologie a neurochirurgie

2007 Číslo 4
-
Všechny články tohoto čísla
- Cervical dystonia
- Repetitive transcranial magnetic stimulation and chronic subjective tinnitus
- Levels of D-dimers in patients with acute ischaemic stroke
- Komentář k pilotní studii autorů D. Školoudíka et al. Změny kognitivních funkcí u pacientů s akutní cévní mozkovou příhodou testovaných pomocí Mini-Mental State Examination (MMSE) a Clock Drawing Test (CDT)
- Changes in congintive functions in patients with acute cerebrovascular event who tested by Mini-Mental State Examination and the Clock Drawing Test
- Decompressive craniectomy as treatment for a rat model of „malignant“ middle cerebral artery infarction
- Correlation of the IgG index and oligoclonal bands in the CSF of patients with multiple sclerosis
- Muscular biopsy in myotonic dystrophy in the era of molecular genetics
- Surgical treatment of hormonally active hypophysial adenomas
- Analysis of 1775 Patients Treated by Percutaneous Radiofrequency Rhizotomy for Trigeminal Neuralgia
- Regulation of mRNA expression of the SMN2 gene by histone deacetylase inhibitors and their influence on the phenotype of type I and II spinal muscular atrophy
- Komentář ke článku Balcer LJ, Galetta SL, Calabresi PA et al. Natalizumab reduces visual loss in patiens with relapsing multiple sclerosis. Neurology 2007; 68: 1299–1304.
- Poliomyelitis-like syndrome caused by tick-meningoencephalitis
- Satelitní anatomický worhshop Transtemporal approaches
- Thrombosis of the sigmoid sinus – current views on diagnosing and treatment
- The treatment of sleep apnea in young children using bilevel positive airway pressure
- Swallowing difficulties in diffuse idiopathic skeletal hyperostosis
- Hennerici MG, Daffertshofer M, Caplan LR, Szabo K (Eds). Case Studies in Stroke. Common and Uncommon Presentations. Cambridge: Cambridge University Press 2007. 272 p. ISBN 0-521-67367-4.
- Lze bez pochybností interpretovat výsledky lumbálního infuzního testu?
- Zpráva z 8. sjezdu Evropské společnosti báze lební
-
Analýza dat v neurologii. IV.
Variabilita měření není vždy „chyba“ - Webové okénko
- XVIII. neuromuskulární sympozium
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle
- Cervical dystonia
- Levels of D-dimers in patients with acute ischaemic stroke
- Thrombosis of the sigmoid sinus – current views on diagnosing and treatment
- Repetitive transcranial magnetic stimulation and chronic subjective tinnitus
