Identification of barriers and benefits of Negative Pressure Wound Therapy
Identifikace bariér a přínosů Negative Pressure Wound Therapy
Cíl: Identifikovat bariéry a přínosy negative pressure wound therapy (NPWT) u pacientů na Chirurgické klinice FN Brno za pětileté období (2017–2021). Soubor a metodika: Retrospektivní, observační deskriptivní studie z dat z nemocničních záznamů pacientů Chirurgické kliniky FN Brno. Výsledky: V průzkumu bylo identifikováno celkem 104 pacientů léčených pomocí NPWT. Průměrný věk pacientů činil 66,7 let (min. věk 27, max. věk 93). Průměrná doba hospitalizace byla 30,2 dní (min. 6, max. 145 dní) a průměrná délka NPWT byla 20,6 dní (min. 4, max. 76 dní). Celkem u 31 pacientů (29,8 %) byla shodná délka hospitalizace a aplikace NPWT a u 27 pacientů (26 %) byl současně zaveden bariérový režim. Etiologie vzniku rány byla různá. Onemocnění gastrointestinálního traktu u 63,4 % (n = 66) pacientů, cévní problematika 33,7 % (n = 35) a dekubitus 2,9 % (n = 3). Frekvence stěru rány byla 4–6 dní a převaz rány (výměna NPWT) byl proveden v intervalu 3–5 dní. U všech pacientů byl využit přístroj VIVANOTec Pro®. Závěry: Z retrospektivní analýzy za 5leté období vyplynulo, že NPWT je využívána u ran různé etiologie, většinou u polymorbidních pacientů vyššího věku. Ve sledovaném souboru nebyly dokumentovány nežádoucí účinky spojené s využitím metody NPWT.
Klíčová slova:
bariéry – podtlaková terapie – retrospektivní analýza – přínosy – negative pressure wound therapy
Authors:
P. Kůřil- 1 3; A. Menšíková 1,2; P. Búřilová 1,2; S. Saibertová 1; A. Pokorná 1
Authors place of work:
Department of Health Sciences, Masaryk University, Faculty of Medicine, Brno
1; Department of Public Health, Masaryk, University, Faculty of Medicine, Brno
2; Department of Surgery, University, Hospital Brno, Brno
3
Published in the journal:
Cesk Slov Neurol N 2022; 85(Supplementum 1): 43-46
doi:
https://doi.org/10.48095/cccsnn2022S43
Summary
Aim: This study aimed to identify barriers and benefits of negative pressure wound therapy (NPWT) in patients at the Department of Surgery of the University Hospital Brno over a five-year period (2017–2021). Methods: Retrospective, observational descriptive study of data from hospital records of patients at the Department of Surgery of the University Hospital Brno. Results: A total of 104 patients who were treated with NPWT were identified in the survey. The mean age of the patients was 66.7 years (Min. age 27, Max. age 93). The mean length of hospitalization was 30.2 days (Min. 6, Max. 145 days) and the mean length of NPWT was 20.6 days (Min. 4, Max. 76 days). In total, 31 patients (29.8%) had the same duration of hospitalization and NPWT application and 27 patients (26%) were simultaneously under a barrier regime. The etiology of the wounds was variable. A gastrointestinal disease in 63.4% (N = 66) of patients, vascular problems in 33.7% (N = 35) and pressure ulcers in 2.9% (N = 3). The frequency of wound swabbing was 4 to 6 days and wound dressing (NPWT) exchange was performed in intervals from 3 to 5 days. The VIVANOTec Pro® device was used in all patients. Conclusion: A retrospective analysis over a five-year period showed that NPWT is routinely used in wounds of various etiologies, mostly in polymorbid patients of older age. No adverse effects associated with the use of NPWT were documented in the study group.
Keywords:
vacuum therapy – benefits – negative pressure wound therapy – barriers – retrospective analysis
Introduction
An effective wound management requires a comprehensive assessment of the patient and wound to determine the most appropriate treatment plan to achieve wound care targets. Several risk factors that can complicate wound healing and increase healthcare costs have been identified [1]. Negative pressure wound therapy (NPWT) has become a widespread method of treatment in a wide range of soft tissue defects over the last 15 years. NPWT is a modern sophisticated method which accelerate the wound healing process, indicated especially in open wounds where is necessary to increase the growth of granulation tissue [2]. The main mechanisms of action in NPWT are indivisibly linked and their interaction promotes healing in many types of wounds. The application of negative pressure causes suction of secretion and detritus from the wound. The cleaned wound base is then ready for example for a final surgical closure [3,4]. NPWT helps to close the wound and prevents a secondary infection. With the help of the local vacuum, cell reproduction activates and a new granulation tissue is formed, which is very necessary for the wound healing process [4,5]. The NPWT method has almost universal applicability and can be used in any medical discipline. In general, NPWT is the most effective for early dehiscence. The sooner NPWT is applied to the wound, the better results of the healing process will be noted [3]. NPWT can be used in various areas of medicine. This method is most often used in surgery, especially in the treatment of partial, but also complete early wound dehiscence, recurrent early seromas, in covering dermo-epidermal grafts, mediastinitis, osteomyelitis of the sternum, trophic ulceration (e. g. pressure ulcers, venous leg ulcers). The use of NPWT is also possible in the treatment of burns (coverage of burns), in dermatovenerology (treatment of ulcerations of various etiologies), for the treatment of diabetic foot syndrome ulcerations and the treatment of wounds after amputation without primary suture of the skin [3,6].
The contraindications of NPWT can be divided into the relative (it requires special preparation and working procedures) and the absolute ones. The relative contraindications include untreated osteomyelitis, the presence of uncovered neurovascular bundle, severe coagulopathy, the presence of parenchymal and hollow organs. The absolute contraindications include an active bleeding, solid necrotic eschars, tumor in the wound bed, and acute soft tissue infections [3,7].
Method
A retrospective, observational descriptive study – case series. The data were extracted from hospital charts from closed medical documentation of patients at the Department of Surgery, University Hospital Brno. The study aimed to identify patients using NPWT according to the reported procedure code 51,850 – wound dressing with NPWT based on controlled negative pressure. The data were analyzed over a five-year period (2017–2021).
Data analysis
Data analysis was performed in IBM SPSS Statistics version 22 Results are presented both as absolute and relative frequencies.
Ethical considerations
The study was performed in compliance with the Helsinki Declaration of 1975 and its subsequent revisions (including the most recent in 2013). The study was not submitted to the ethics committee approval, patients have signed the informed consent for hospitalization, and the data were not collected with direct patient participation. All data were extracted from medical records and anonymized.
Results
In the determined period from 2017 to 2021, a total of 104 patients (100%) were treated with NPWT at the Department of Surgery, University Hospital Brno. In the study cohort, 43.3% (N = 45) of women and 56.7% (N = 59) of men were included. The average age of patients was 66.7 years (Min. age 27, Max. age 93). The mean length of the hospital stay was 30.2 days (Min. 6, Max. 145 days) and the mean duration of NPWT was 20.6 days (Min. 4, Max. 76 days). For the cumulative number of days of hospitalization and the number of days of NPWT application. In total, 31 patients (29.8%) had the same length of hospitalization and NPWT application. In 27 patients (26%), a barrier regime was used at the same time (potentially dangerous bacterial strains of group B in 24 patients, group C in three patients). The etiology of the wounds was different. Gastrointestinal tract (GIT) disease in 63.4% (N = 66) of patients, vascular problems in 33.7% (N = 35), and pressure ulcers in 2.9% (N = 3). The frequency of wound swabbing varied from 4 to 6 days and wound dressing (NPWT) exchange was performed in intervals from 3 to 5 days. The VIVANOTec Pro® (The company HARTMANN – RICO a. s., Czech Republic – Veverská Bitýška) device was used in all patients.
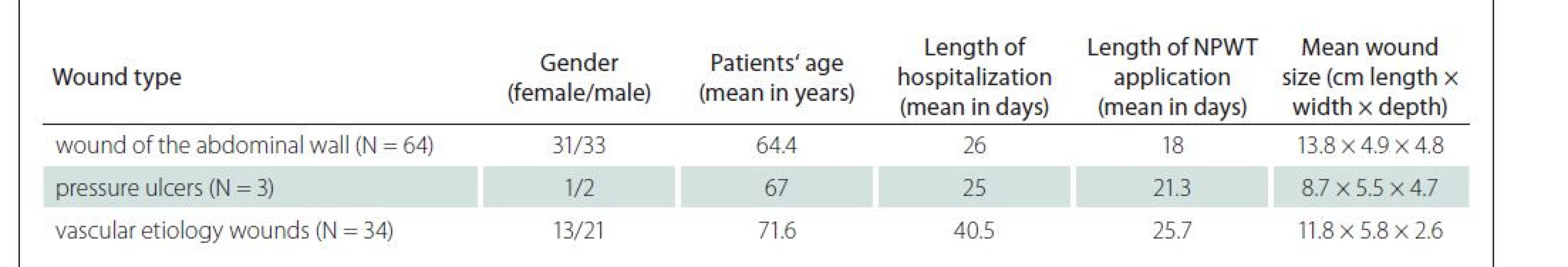
Application of NPWT to the abdominal wall defects
In 64 cases (31 females and 33 males) where NPWT was applied to the abdominal wall, wound closure was achieved by secondary (delayed) suture. The mean age of the patients was 64.4 years (Min. age 27, Max. age 93), the mean hospital stay was 26 days (Min. 8, Max. 88), and the mean duration of NPWT application was 18 days (Min. 4, Max. 46). The most common etiologies of the wounds in GIT diseases were dehiscences in complicated abdominal surgeries, after acute abdominal disorders, after peritonitis and in patients with cancer. In three cases, the dehiscence of both ends of the laparotomy was bridged with a sponge.
Application of NPWT in patients with pressure ulcers
Pressure ulcer (PU) was treated with NPWT in three cases (1 female and 2 males). The mean age of the patients was 67 years (Min. age 46, Max. age 91), the mean duration of NPWT application was 21.3 days (Min. 10, Max. 28) and the mean hospital stay was 25 days (Min. 14, Max. 33). One case was a PU in category III of the left gluteal region in the area of the anus (wound size – length x width x depth: 3 x 2.5 x 5 cm). In the second case, the PU was in category IV on the sacrum with a subsequent extirpation of coccygeal bone (wound size: 15 x 6 x 4 cm). Wound closure was achieved in both cases. The third patient with PU of category IV on the sacrum (wound size 8 x 8 x 5 cm) was almost fully healed with NPWT. On demand of the family, the patient was transferred to home care and the moist wound healing method was further applied.
Application of NPWT in wounds of vascular etiology
In 34 cases (13 women and 21 men), NPWT was indicated for treatment of wounds of vascular etiology. The mean age of the patients was 71.6 years (Min. age 49, Max. age 88), the mean hospital stay was 40.5 days (Min. 12, Max. 145) and the mean duration of NPWT was 25.7 days (Min. 7, Max. 55). The most common wound origins with vascular etiologies were diabetic ulcerations, vascular occlusions, and reconstructive vascular procedures in ischemic lower limb disease. After a consultation with the Department of Burns and Plastic Surgery, wound closure with a split thickness skin graft was performed in two patients and wound closure with autograft was planned in six patients. In one case, NPWT was applied on the wound after fasciotomy of the arm and forearm of the right upper limb in a patient with obliteration of the right subclavian artery, which resulted in the right upper limb palsy due to the compartment syndrome. The 21 x 2.5 x 2 cm wound was treated with NPWT for 14 days and then resutured. The total length of hospitalization in the 66-year--old man was 21 days. In two male patients, NPWT was applied in the rectum and buttocks region. The first patient (62 years old, length of hospitalization and NPWT was 13 days) had NPWT placed in the gluteal area (wound size of left buttock 10 x 6 x 5 cm, right buttock 7 x 4 x 4 cm) for an abscess in the field of recurrent pilonidal sinus. The other man (50-years-old, length of hospitalization 39 days and duration of NPWT 29 days) had NPWT placed in the rectal area (wound size 6 x 4 x 5 cm) for ischemia of the coloanal anastomosis. In both patients wound closure was achieved. Tab. 1 summarizes the information about the group of patients mentioned above.
Discussion
The NPWT method is described as an effective tool in treatment of wounds of various etiologies and is nowadays commonly indicated in the treatment of open abdominal lacerations, sternal wound complications after cardiac surgery and complex non-healing wounds. Although the clinical use of NPWT is widespread, the high-level evidence of its efficiency and economic benefits are still insufficient [8–10]. Data analysis in the conducted study verified that NPWT is beneficial in a different spectrum of wound etiology. In all cases studied, the wound healing process was positively affected and no adverse effects related to the use of NPWT were found. The care of pressure lesions using NPWT is relatively well documented. There are recommendations for the treatment depending on the category and seriousness of the pressure ulcers. For categories I and II, a conservative, non-surgical approach may be appropriate. Pressure ulcers in categories III and IV usually require surgical treatment [8,11,12]. Optimal preoperative and postoperative care is crucial in preventing recurrences [13]. The results of studies have identified several potential benefits in the NPWT method for category III and IV, including enhanced exudate management, increased tissue perfusion of the wound, stimulation of granulation tissue formation, and decreased bacterial load [14]. In addition, studies have shown positive results in the treatment of early complications after arterial revascularization in the lower limbs and the management of limited infection of the vascular prosthesis [15]. The aforementioned literature sources confirm the positive findings and outcomes in the patients observed in the present study.
Thus, NPWT allows not only new clinical approaches but also has an impact on the economic costs of wound treatment, in the described examples primarily concerning the duration of hospitalization. Regarding many other factors, including less frequent dressing changes, shortening of the duration of treatment, acceleration of the healing process and reduction of the length of hospital stay, cost savings have been noticed with the use of NPWT [16].
Conclusion
Our retrospective analysis and case study aimed to identify barriers and benefits of NPWT in a group of patients at the Department of Surgery, University Hospital Brno. The retrospective analysis over a 5-year period showed that NPWT is used in wounds of different etiology, mostly in elderly patients with multiple comorbidities. As the main benefits recognized based on our analyses should be mentioned there was no adverse effects associated with NPWT documented in the observed group. A potential barrier to the appropriate NPWT use is the still ambiguous recommendations for its use, which is a problem not at the above-mentioned department. Further research activities aim to standardizing NPWT procedures and processes, including evaluation of its efficacy.
Acknowledgments
The authors thank all the staff of the Department of Surgery, University Hospital Brno for providing the data to realize this study.
Dedication
This study was written at Masaryk University as a part of the project „A comprehensive approach to skin and mucosal integrity disorders II.“ number MUNI/A/1341/2021 with the support of the Specific University Research Grant, as provided by the Ministry of Education, Youth and Sports of the Czech Republic in the year 2021.
Conflict of interests
The authors declare that they have no commercial interests in relation to the subject of the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
PhDr. Petra Búřilová, BBA
Department of Health Sciences
Faculty of Medicine
Masaryk University
Kamenice 3
625 00 Brno
e-mail: burilova@med.muni.cz
Zdroje
1. Orgill DP, Bayer LR. Negative pressure wound therapy: past, present and future. Int Wound J 2013; 10 (Suppl 1): 15–19. doi: 10.1111/iwj.12170.
2. Kim PJ, Attinger CE, Steinberg JS et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 2014; 133 (3): 709–716. doi: 10.1097/01.prs.0000438060.46290.7a.
3. Šimek M, Bém R. Podtlaková léčba ran. Praha: Maxdorf 2013.
4. Pokorná A. Úvod do wound managementu. Příručka pro hojení ran pro studenty nelékařských oborů. Brno: Masaryk University 2012.
5. Iheozor-Ejiofor Z, Newton K, Dumville JC et al. Negative pressure wound therapy for open traumatic wounds. Cochrane Database Syst Rev 2018; 7 (7): CD012522. Doi: 10.1002/14651858.CD012522.pub2.
6. Webster J, Liu Z, Norman G et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev 2019; 3 (3): CD009261. Doi: 10.1002/14651858.CD009261.pub4.
7. Beitz J, Rijswijk L. Developing evidence-based algorithms for negative pressure wound therapy in adults with acute and chronic wounds: literature and expert-based face validation results. Ostomy Wound Manage 2012; 58 (4): 50–69.
8. Kim PJ, Attinger CE, Constantine T et al. Negative pressure wound therapy with instillation: international consensus guidelines update. Int Wound J 2020; 17 (1): 174–186. doi: 10.1111/iwj.13254.
9. Campbell PE, Smith GS, Smith JM. Retrospective clinical evaluation of gauze-based negative pressure wound therapy. Int Wound J 2008; 5 (2): 280–286. doi: 10.1111/j.1742-481X.2008.00485.x.
10. Norman G, Goh EL, Dumville JC et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev 2020; 6 (6): CD009261.doi: 10.1002/14651858.CD009 261.
11. Matiasek J, Djedovic G, Kiehlmann M et al. Negative pressure wound therapy with instillation: effects on healing of category 4 pressure ulcers. Plast Aesthet Res 2018; 5 : 36. doi: 10.20517/2347-9264.2018.50.
12. Dumville JC, Webster J, Evans D et al. Negative pressure wound therapy for treating pressure ulcers. Cochrane Database Syst Rev 2015; 5: CD011334. doi: 10.1002/14651858.CD011334.pub2.
13. Hokýnková A, Šín P, Černoch F et al. Využití lalokových plastik v operační léčbě dekubitů. Cesk Slov Neurol N 2017; 80/113 (Suppl 1): S41–S44. doi: 10.14735/amcsnn2017S41.
14. Mervis JS, Phillips TJ. Pressure ulcers: prevention and management. J Am Acad Dermatol 2019; 81 (4): 893–902. doi: 10.1016/j.jaad.2018.12.068.
15. Rezk F, Åstrand H, Acosta S. Incisional negative pressure wound therapy for the prevention of surgical site infection after open lower limb revascularization – rationale and design of a multi-center randomized controlled trial. Contemp Clin Trials Commun 2019; 16 : 100469. doi: 10.1016/j.conctc.2019.100469.
16. Apelqvist J, Willy C, Fagerdahl AM et al. EWMA document: negative pressure wound therapy. J Wound Care 2017; 26 (Suppl 3): S1–S154. doi: 10.12968/jowc.2017.26.Sup3.S1.
Štítky
Dětská neurologie Neurochirurgie NeurologieČlánek vyšel v časopise
Česká a slovenská neurologie a neurochirurgie

-
Všechny články tohoto čísla
- Skin grafting in surgical treatment of pressure ulcers
- The use of negative pressure wound therapy in a selected medical facility
- Monitoring the prevalence of pressure ulcers – a comparison of national data with data of a specific health care provider – University Hospital Ostrava
- The use of incontinence devices and urinary/ faecal diversion management devices in hospitalised patients as a possible cause of unwanted immobilization
- Can different type of the pressure ulcers debridement affect oxidative stress parameters?
- Nurses‘ knowledge in the field of specific prevention and treatment of heels pressure injuries
- Identification of barriers and benefits of Negative Pressure Wound Therapy
- Standardization of wound care for patients in Austria, Germany and Slovakia
- Determiners of pressure ulcers formation – analyses from hospital information system
- Advanced practice nursing in the field of wound management
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle
- Nurses‘ knowledge in the field of specific prevention and treatment of heels pressure injuries
- Monitoring the prevalence of pressure ulcers – a comparison of national data with data of a specific health care provider – University Hospital Ostrava
- Standardization of wound care for patients in Austria, Germany and Slovakia
- Advanced practice nursing in the field of wound management
